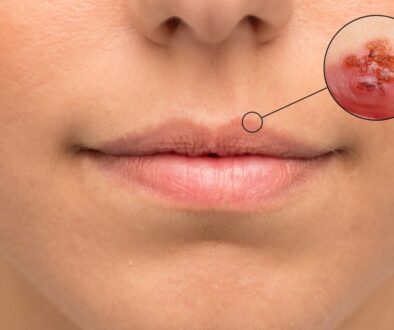
Do I have a cold sore?
What is a cold sore?
Cold sores are caused mainly by two herpes simplex viruses (HSVs): herpes simplex-1 (HSV-1) and herpes simplex-2 (HSV-2) (HSV-2). The majority of oral herpes infections are caused by HSV-1, which is most frequently spread through saliva; the majority of genital herpes infections are caused by HSV-2, which is found in vaginal fluids. Orogenital contact, on the other hand, may result in a primary infection of either kind in the oral or genital area. HSV-1 and HSV-2 both have the potential to produce primary or recurrent infections. When a first infection is symptomatic and involves the oral area, it is referred to as primary herpes gingivostomatitis. Although not always, 20–40% of individuals who acquire a first herpes infection develop later recurrent herpes infections as a result of HSV reactivation from dormant cerebral ganglion cells. Oral recurrences often affect the vermilion border of the lips and are referred to as herpes labialis, cold sores, or fever blisters. Recurrences occur less often on the hard palate, chin, or oral mucosa.
Around one-third of school-aged children have primary HSV-1 infection , and up to 80% of adolescents and adults have serological evidence of HSV-1 infection. Babies often receive anti-HSV antibodies from their mothers, which protect them against infection until they reach the age of approximately six months. HSV-1 may be spread via close oral-to-oral contact and through contact with virus-infected sores, saliva, and mouth surfaces. Transmission may occur when infected individuals share cosmetics, razors, towels, or dining utensils. After sexual activity starts, the likelihood of HSV-2 infection rises, with risk factors including being female, having a history of sexually transmitted illness, and having numerous sexual partners.
Prevention
Emotional stress, tiredness, sun exposure (UV light), menstruation and other hormonal changes, fever, heat, upper respiratory tract infection, tooth extraction, and physical trauma or surgery are all common stressors that may trigger recurrences.
Take the following preventive steps into consideration:
Reduced stress (e.g., healthy diet, enough sleep and exercise, and use of relaxation methods) may help avoid recurrences in people for whom stress is a recognized trigger.
In people who report more than one incident per year, prophylactic antiviral therapy prior to dental operations may be recommended to avoid recurrence.
Sun protection, particularly at the beach and on ski slopes, may likely decrease the frequency of cold sore recurrences.
30 minutes before to sun exposure, apply a sunscreen with an SPF of 30 or higher on the lips and face.
By frequently washing your hands and avoiding skin-to-skin contact with others until the blister has dried and crusted over, you may prevent the spread of cold sores to other areas of your body and to other people.
Nonpharmacological Treatment
Advise patients to clean the lesion gently with a moderate soap and water solution. Alternatively, cold tap-water compresses may be applied to the region. To minimize autoinoculation and the spread of HSV, patients should avoid excessive touching of the lesion and regularly wash their hands.
Heat application is a therapy that has not been tested in randomized trials. Lipstick-shaped devices have been offered for use on regions experiencing prodromal symptoms. The high temperature (50°C) is hypothesized to alleviate the intensity of symptoms such as burning, blistering, itching, and swelling, perhaps by inhibiting viral multiplication.
Pharmacologic Treatment
In immunocompromised individuals, oral HSV infections are self-limiting. Analgesics may be prescribed to alleviate symptoms, and topical protectants may help prevent the lesions from cracking and drying excessively (e.g., allantoin, calamine, cocoa butter, petrolatum, zinc oxide). Antivirals may be prescribed to immunocompetent individuals who benefit from a reduction in the duration of symptoms. Patients who are immunocompromised should be referred to a qualified health care practitioner for further assessment. The following table summarizes the most often prescribed medicines for the treatment of cold sores.
Analgesics
For a period of no more than three days, systemic analgesics such as acetaminophen, ibuprofen, or naproxen may be suggested to manage moderate to severe pain. Topical anesthetics such as benzocaine, camphor, lidocaine, menthol, phenol, pramoxine, or prilocaine may be beneficial in temporarily alleviating moderate discomfort. The dosages that are most often utilized are shown in Table 1.
Antivirals
Without antiviral therapy, the anticipated duration for a cold sore to recover naturally is 7–10 days. Docosanol is a topical drug that inhibits the transmission of the herpes simplex virus to healthy cells. Acyclovir, famciclovir, and valacyclovir have all been investigated for the treatment and prevention of cold sores; however, only valacyclovir is approved by Health Canada for the treatment of cold sores in individuals over the age of 12 years. While oral acyclovir is not officially recommended for the treatment of herpes labialis, it is the only antiviral drug authorized for usage in adults and children (>2 years). Valacyclovir and famciclovir (prodrugs of acyclovir and penciclovir, respectively) enhance the bioavailability of their active forms. In general, these antiviral medicines have minimal harmful effects since they are transformed to active drug only after they reach virally infected cells through viral thymidine kinase.
Treatment of primary infections with antivirals
Antiviral therapy is often suggested for uncomplicated bouts of primary oral herpes in healthy individuals in moderate and severe cases. Treatment is most successful when started promptly, preferably within 72 hours. In a small randomized controlled study in children, oral acyclovir reduced the duration of symptoms (e.g. fever, odynophagia, lesions) and viral shedding when compared to placebo. Although randomized controlled studies are limited, famciclovir and valacyclovir are acceptable therapeutic options. Typically, therapy lasts seven days but may extend to ten days depending on the severity of symptoms and response to treatment.
Treatment with antivirals for recurring infections
Three distinct strategies for antiviral therapy of recurring infections are possible:
Intermittent episodic therapy (IET) is used to treat isolated, acute HSV infections at the onset of any clinical sign or symptom associated with a primary or recurring infection. Oral acyclovir famciclovir, and valacyclovir are all recommended. Antiviral regimens with high doses and a short duration of action are used to treat recurrent infections. In patients with prodromal symptoms, treatment should begin as soon as feasible, preferably within 48 hours. Acyclovir, famciclovir, and valacyclovir have been demonstrated in randomized controlled studies to reduce the time required for lesion healing and the duration of symptoms by 1–2 days. In comparison to acyclovir, valacyclovir significantly lowers the time required for healing and pain resolution in recurring infections. Famciclovir and valacyclovir are more convenient for patients due to their shorter treatment duration and less frequent dosage, as well as their lower total cost when compared to acyclovir.
Additionally, the data supports the use of topical acyclovir 5% cream alone or in combination with topical hydrocortisone for recurring infections.
However, topical antivirals seem to be less successful in reducing the time required for healing than systemic therapies.
Docosanol is a topical cold sore therapy with a modest clinical effect. Docosanol should be administered five times daily, as soon as discomfort, itching, burning, redness, or tingling occur. When docosanol was compared to a placebo (polyethylene glycol) in a randomized controlled trial, it was discovered that docosanol healed 17 hours faster (4.1 days vs. 4.8 days) and alleviated discomfort 12 hours faster (2.2 days vs. 2.7 days) when the creams were applied five times daily, with the first application within 12 hours of episode onset. Because the time to recovery in the placebo group was likewise substantially shorter than the anticipated natural healing period, the possibility of the polyethylene glycol vehicle having a therapeutic impact has been raised.
Chronic suppressive treatment (CST) is not recommended for the majority of patients with HSV infection, but may be suitable for the 5–10% who have recurrent recurrences (6 per year) and also have deformity, trouble swallowing or significant discomfort, protracted episodes, or are especially disturbed.
The use of low-dose daily oral acyclovir, valacyclovir, or famciclovir is supported by evidence. It is not advised to utilize topical treatment during CST.
Intermittent suppressive treatment (IST) is indicated when recurrences are expected as a result of known triggering events (see Prevention), especially in circumstances where reducing virus shedding reduces the probability of infecting seronegative people.
Although specific dosage recommendations for IST are not available, extrapolation of data from CST trials is considered acceptable. Oral acyclovir has been found to be effective in reducing recurrences caused by sunlight; however, results on topical acyclovir cream are inconsistent (possibly due to poor penetration from site of application).
Corticosteroids
Corticosteroids are not usually advised for the treatment of viral-induced oral inflammation, since they may conceal the spread of infection and inhibit the natural immune response. Their topical use (e.g., fluocinonide 0.05 percent, hydrocortisone 1%) in combination with antivirals, however, may be beneficial.
Natural Health Supplements
There is some evidence that applying a cream of lemon balm (Melissa officinalis) containing 1% of a 70:1 leaf extract to the site of a cold sore during the prodromal stage decreases the number and size of lesions, but does not diminish the intensity of the outbreak.
[Lemon balm is often used twice daily from the beginning of the prodrome, preferably within 72 hours, until a few days after the lesions have healed, i.e., 5–10 days.
For the prevention and treatment of cold sores, lysine, an important amino acid, is available in oral and topical dose forms. Lysine is thought to have an antiviral impact by competing with arginine, another important amino acid needed for viral reproduction. The evidence supporting lysine’s efficacy in this indication is inconsistent, with some research suggesting that efficacy is dose-dependent.
Additional Therapies
Zinc formulations used topically have been found to help individuals with cold sores and may speed up the healing process when given as soon as symptoms begin.
[48] There is a possibility that the risk of skin irritation may be enhanced. Further information is needed due to the absence of uniform frequency and concentration, the diversity of zinc salts used in studies, and the scarcity of high-quality data.
When used for a 3–4 month treatment term, limited data indicates that daily oral zinc sulfate (up to 50 mg/day) may decrease the incidence of cold sores and the length of lesions during an episode.
However, it is worth noting the possibility of copper insufficiency associated with long-term zinc usage and the scarcity of high-quality evidence.
There is no documented data supporting the safety and efficacy of heparin in the treatment of cold sores, despite the fact that it is an often suggested component.
Caustic chemicals, such as silver nitrate, may aggravate cold sores and should not be used.
Topical medicines that are very astringent, such as tannic acid, are not suggested for the treatment of cold sores. They have the ability to dry out the region excessively, resulting in fissures, pain, and the possibility of bacterial superinfection.