Syphilis is Making a Comeback: Here’s What You Need to Know
Syphilis, a sexually transmitted infection (STI) that has been around for a long time, is making a troubling return globally, particularly in Canada. The significant increase in cases, with adult instances quadrupling and congenital cases tripling, requires urgent action. It is crucial to raise awareness about syphilis in order to prevent its spread and avoid serious health consequences.
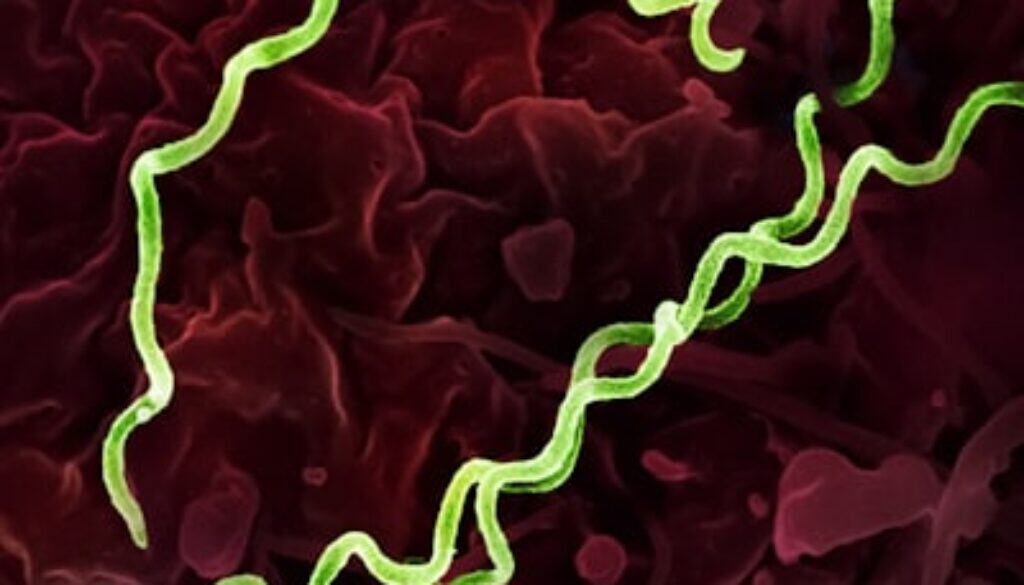
Understanding Syphilis: The Basics
As the infection progresses without treatment, secondary symptoms emerge. These include:
- Unusual rashes that can appear anywhere on the body, including the palms of the hands and soles of the feet.
- Flu-like symptoms such as fever, fatigue, sore throat, and swollen lymph nodes.
These signs may also resolve spontaneously, leading many to believe the infection has cleared. However, this leads directly into the latent syphilis phase. During latency, the bacteria remain hidden deep inside the body without any visible symptoms.
This dormant period poses significant danger: although symptoms disappear, the bacteria continue to cause damage internally. If untreated, syphilis can reemerge years later with severe health consequences affecting vital organs such as the heart and brain.
Recognizing these early syphilis symptoms — painless bump, rash, flu-like signs — is critical for timely testing and treatment before entering latent stages where detection becomes more difficult and risks increase dramatically.
Why Syphilis is Making a Comeback
Data from Canada reveals a concerning trend in syphilis cases:
- Quadrupling of Adult Cases: The number of adult syphilis cases has increased fourfold, indicating a significant rise in infections among the population.
- Tripling of Congenital Cases: Cases of congenital syphilis in babies have also tripled, highlighting the impact on future generations.
Factors contributing to this resurgence include:
- Decreased Condom Use: With changing sexual health trends, there has been a decline in consistent condom usage, leading to higher transmission rates of STIs like syphilis.
- Multiple Sexual Partners: Engaging in sexual activities with multiple partners increases the risk of exposure to syphilis and other STIs.
- Lack of Awareness: A general lack of awareness about syphilis, its symptoms, and the importance of safe sexual practices has contributed to its resurgence.
- Stigma Surrounding STIs: The stigma associated with sexually transmitted infections can prevent individuals from seeking timely testing and treatment, further fueling the spread of syphilis.
Recognizing vulnerable populations and high-risk behaviors is crucial in addressing this public health concern. By understanding the root causes behind the rising syphilis rates and implementing targeted interventions, we can work towards curbing this alarming comeback.
Risks and Complications of Untreated Syphilis
Untreated syphilis poses significant risks and complications, especially when considering its resurgence in recent years. Here are the key points to be aware of:
1. Congenital Syphilis
Untreated syphilis in pregnant women can lead to the transmission of the infection to their unborn babies, resulting in serious consequences such as miscarriages, stillbirths, and developmental issues like bone deformities and liver complications.
2. Long-Term Health Risks
For infected individuals who do not seek timely treatment, syphilis can silently cause severe internal damage over time. The bacteria can affect various organs and systems in the body, leading to long-term health complications if left unchecked.
It is crucial to understand the gravity of these risks associated with untreated syphilis, particularly in the context of its resurgence. Early detection and prompt treatment are essential in preventing these severe outcomes.
Prevention Strategies to Protect Yourself and Your Baby
Taking proactive steps is crucial in protecting yourself and your baby from the risks associated with syphilis. Here are some effective prevention strategies:
1. Consistent Use of Barrier Protections
Using barrier protections such as condoms consistently and correctly is one of the most effective ways to reduce the risk of contracting syphilis and other sexually transmitted infections (STIs). This is especially important if you have multiple sexual partners. Condoms act as a physical barrier, preventing direct contact and reducing the chances of transmission.
2. Prompt Testing After Potential Exposure
If you believe you may have been exposed to syphilis or any other STI, it is essential to get tested promptly. Timely testing allows for early detection and treatment, which can prevent further transmission and complications. Speak with your healthcare provider about the appropriate tests and when to get them done.
3. Pre-Exposure Prophylaxis Options for High-Risk Groups
For individuals at high risk of exposure to syphilis, such as men who have sex with men or those with multiple sexual partners, pre-exposure prophylaxis (PrEP) options may be available. Doxycycline, an antibiotic medication, can be taken within 72 hours after a risky encounter to help lower the chances of syphilis infection. Consult with your healthcare provider to determine if this preventive measure is suitable for you.
4. Prenatal Screening for Pregnant Women
Regular prenatal screening during pregnancy is vital in preventing congenital syphilis, which can cause severe harm to the unborn baby. Pregnant women should undergo routine testing for syphilis as part of their prenatal care. If detected early, appropriate treatment can be administered to protect both the mother and the baby.
By implementing these prevention strategies, individuals can take control of their sexual health and contribute to reducing the spread of syphilis. Prioritizing protection methods, regular testing, and appropriate preventive measures plays a significant role in safeguarding oneself and their babies from the risks associated with this resurging STI.
Diagnosis and Testing for Syphilis: What You Need to Know
Syphilis testing methods primarily involve blood tests that detect antibodies produced in response to the infection. These tests are essential because the initial symptoms—like painless bumps or rashes—can be subtle or mistaken for other conditions.
Key syphilis testing methods include:
- Nontreponemal tests (e.g., RPR or VDRL): Screen for general antibodies indicating infection.
- Treponemal tests (e.g., FTA-ABS, TPPA): Confirm presence of syphilis-specific antibodies, used after positive screening.
Early testing during pregnancy is critical to prevent congenital syphilis. Pregnant individuals undergo screening as part of routine prenatal care, with repeated testing recommended if they belong to high-risk groups or have ongoing exposure risks.
Anyone suspecting exposure should seek medical evaluation without delay. Rapid identification allows timely treatment, reducing risks of complications and transmission. Clinics and pharmacies in urban centers like Toronto offer accessible testing services—no need to wait.
Prompt testing supports early diagnosis, enabling effective treatment plans tailored to individual needs. Testing also plays a pivotal role in public health efforts to control the resurgence of syphilis by identifying infections before they cause severe damage or spread further.
Effective Treatment Options for Syphilis Infections
Syphilis is Making a Comeback! Prompt and effective treatment is essential to stop its progression and prevent serious health consequences.
Standard Treatment: Penicillin Therapy
- The cornerstone of syphilis treatment is Bicillin (benzathine penicillin G).
- Typically administered as one or more intramuscular injections, often described as “one shot in each butt cheek.”
- Penicillin remains the most effective antibiotic against syphilis bacteria.
- Especially critical for pregnant women, where penicillin treatment syphilis is the only recommended option to protect both mother and baby.
Alternative Treatment: Doxycycline
- For individuals allergic to penicillin, an oral doxycycline regimen offers an alternative.
- Usually prescribed as doxycycline 200 mg daily for 14 days.
- Not suitable for pregnant women due to potential risks to fetal development.
- Close medical supervision required when using doxycycline to ensure effectiveness.
Treatment success depends on timely administration. Delaying therapy allows the bacteria to advance through stages that cause irreversible damage. Patients should complete the full course and follow up with healthcare providers for monitoring.
Clear understanding of these options empowers those affected. Proper treatment interrupts transmission chains—protecting you, your partners, and future generations from this resurging threat.
Managing Treatment Side Effects and Post-Treatment Care for Syphilis Patients
Explanation of common side effects
After antibiotic treatment for syphilis, patients may experience the Jarisch-Herxheimer reaction. This reaction occurs due to the rapid killing of bacteria by the antibiotics, leading to the release of toxins into the bloodstream as the bacteria die off.
The Importance of Partner Notification and Testing in Controlling Syphilis Outbreaks
When it comes to controlling syphilis outbreaks, one key strategy is ensuring that sexual partners are tested for the infection. This is crucial in preventing reinfection cycles and breaking the chain of transmission. Here’s why partner notification and testing are so important:
Why Partner Testing Matters
- Preventing Reinfection: If one partner is treated for syphilis but the other remains untreated, there’s a high risk of reinfection. By testing both partners simultaneously, we can ensure that both individuals receive appropriate treatment and reduce the chances of spreading the infection further.
- Breaking the Chain of Transmission: Syphilis is primarily transmitted through sexual contact. By identifying and treating infected individuals, we can interrupt the transmission cycle and prevent new cases from occurring. Partner testing plays a vital role in this process by identifying potential sources of infection.
- Promoting Safe Sexual Practices: Partner notification and testing provide an opportunity to educate individuals about safe sexual practices. By encouraging open communication between partners about their sexual health, we can promote condom use and reduce the risk of STIs, including syphilis.
Implementing Partner Notification and Testing
To effectively control syphilis outbreaks, healthcare providers should prioritize partner notification and testing as part of their intervention strategies. Here are some key steps:
- Encouraging Open Communication: Healthcare providers should create a supportive environment where patients feel comfortable discussing their sexual history and informing their partners about potential exposure to syphilis.
- Providing Resources: It’s essential to provide resources such as brochures or online materials that explain the importance of partner testing and offer guidance on how to approach conversations with partners.
- Collaborating with Public Health Agencies: Healthcare providers can work closely with public health agencies to ensure that partner notification efforts are coordinated and that resources are allocated effectively.
By prioritizing partner notification and testing, we can enhance our efforts in controlling syphilis outbreaks and protecting the sexual health of individuals within our communities.
Protecting Future Generations from Congenital Syphilis
Syphilis is Making a Comeback! This resurgence poses a serious threat to newborns through congenital syphilis. Babies born to infected mothers undergo immediate testing after birth to detect any infection early. Prompt diagnosis allows for rapid intervention, often involving a 10-day course of intravenous antibiotics to eliminate the bacteria completely. These protocols are critical in congenital syphilis prevention, reducing risks of devastating outcomes such as miscarriages, stillbirths, and developmental complications affecting bones and liver. Vigilant screening and treatment at birth safeguard infants’ health and interrupt the cycle of transmission.
Breaking the Silence Around Syphilis: Reducing STI Stigma Through Public Health Education
STI stigma reduction is critical for effective syphilis control. Shame and fear create barriers to seeking timely medical care and openly discussing risks. When people hesitate to get tested or disclose symptoms, infections spread silently.
Public health education must:
- Normalize conversations around syphilis and other STIs
- Emphasize that infection is a medical issue, not a moral failing
- Encourage prompt testing and treatment without judgment
Removing stigma empowers individuals to protect themselves and their partners. Honest dialogue fuels early detection, preventing severe health outcomes and breaking the cycle of transmission.
Conclusion
Syphilis is making a comeback. Action is urgent. Protect yourself and your loved ones with these simple, effective steps:
- Use protection consistently, especially with multiple partners.
- Get tested regularly if you are sexually active, pregnant, or belong to high-risk groups.
- Seek prompt medical care if exposure is suspected.
- Encourage prenatal screening to prevent congenital syphilis.
- Share this knowledge widely. Awareness saves lives.
“Get tested. Stay healthy. Syphilis awareness prevention tips matter now more than ever.”
The rise in syphilis cases demands vigilance. Early detection and treatment break the chain of transmission. Your health matters — taking these precautions today helps curb this silent epidemic tomorrow.